All About Liver Transplant and Surgery
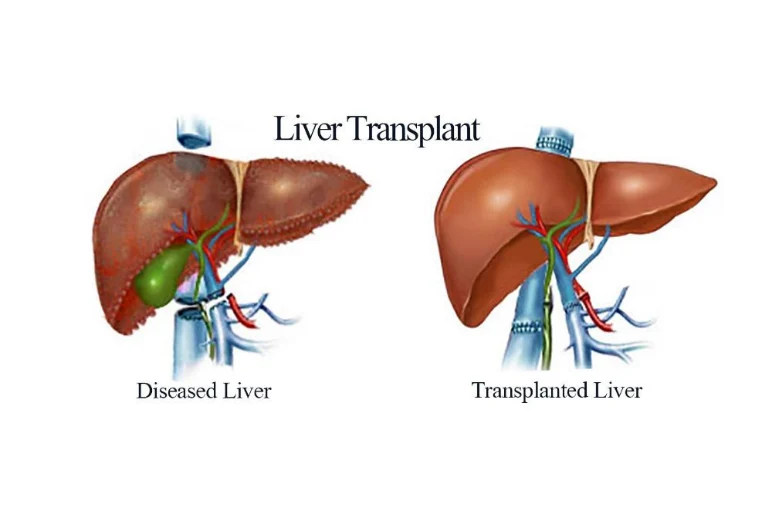
A liver transplant is a surgical procedure used to replace a failing liver from one person’s body with a healthy one from another. You have the option of receiving a portion of a liver from a living donor or the entire liver from a donor who was just declared deceased. A split liver can regrow to its original size in both your body and the body of the living donor.
A liver transplant is a life-saving operation that requires a highly trained and experienced surgeon above all else, as well as a hospital with state-of-the-art facilities to carry out this intricate and significant surgery.
What is the Need for Liver Transplant
A variety of acute and chronic conditions can impact the proper functioning of the liver, necessitating liver transplants. This option is typically extended to individuals with end-stage liver disease who may prove unresponsive to alternative treatments. Listed below are some analogous conditions:
Acute Liver Failure (Fulminant Hepatic Failure): This rapid loss of liver function, occurring over days or weeks, is known as acute liver failure. Typically, it affects individuals without pre-existing liver disease.
Viral Hepatitis: An infection causing inflammation or damage to the liver is referred to as viral hepatitis.
Alcoholic Liver Disease: Resulting from alcohol consumption, this condition damages the liver, leading to fat accumulation, inflammation, and scarring. Alcoholic liver disease can be fatal.
Non-Alcoholic Fatty Liver: Characterized by the accumulation of fat in the liver, this condition can progress to inflammation and scarring.
Primary Liver Cancer: Occurring when cancerous growths develop in the liver, primary liver cancer necessitates various treatments, including chemotherapy, radiation therapy, partial liver removal, and transplantation.
Diagnosis & Evaluation
Upon the diagnosis of end-stage liver disease, a liver specialist typically recommends an evaluation process that unfolds in three stages, typically spanning 5-7 days of hospitalization.
Diagnostic and Severity Assessment: This stage aims to establish a definitive diagnosis, evaluate the severity of liver disease, and determine the urgency of transplantation.
Fitness Evaluation for Transplantation: The patient’s suitability for transplantation is assessed by examining other systems such as the heart, lungs, kidneys, and blood counts. Any presence of infection is ruled out, and the liver specialist gauges the likelihood of surgical success based on the patient’s overall condition and the cause and severity of liver disease.
Mental and Psychological Preparation: The final stage involves preparing the patient mentally and psychologically. Counseling sessions for patients and their families cover details about the procedure, expected hospital stay, potential postoperative course, follow-up, and aftercare.
After the evaluation, the patient is either added to the waiting list for a donor liver or, if a willing and blood group-matched family donor is available, the patient undergoes evaluation for donation, and a transplant is scheduled.
While on the waiting list for a cadaver donor, the patient maintains regular follow-ups with the transplant team until a suitable liver becomes available. In cases of deterioration, consideration may be given to a living liver donation within the family.
Life after Liver Transplant
Liver transplantation can significantly enhance a patient’s quality of life, but adherence to certain practices is crucial for leading a normal life post-transplant.
Regular Follow-Up: In addition to visits with surgeons and doctors, consistent follow-ups with the transplant team, including psychological specialists, are advised for the first few months post-transplant. These visits help monitor the body’s response to the transplant and address any potential complications.
Immunosuppressants: To prevent rejection, immunosuppressant drugs are often prescribed, as the body has a tendency to reject foreign substances.
Hygiene and Lifestyle: Embracing good hygiene practices and maintaining an active lifestyle contribute significantly to recovery. A healthy routine involving physical activity, a balanced diet, and avoidance of smoking is encouraged. Alcohol consumption is strictly discouraged, and dietary plans may be customized with the guidance of a dietitian.
Survival Rate: The one-year post-surgery survival rate is reported to be between 88-90%.







